3 D Printing for Vascular Diseases
By Pamela Marcucci
Imagine a 3D printer helping to better treat diseases involving the heart and the brain. That is exactly what the Jacobs Institute (JI) is doing with Kaleida Health’s Gates Vascular Institute and the University at Buffalo’s Clinical and Translational Research Center.
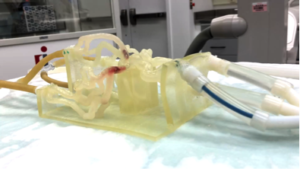
The newest technology for treating vascular diseases, 3D printing is helping build three-dimensional models one layer at a time. Starting with one layer and bonding it with another thin layer of material, biomedical engineers are building flow models that mimic patients’ brain and heart vasculatures. After undergoing an MRI or CT scan, a patient’s anatomy is segmented out in the images, and sent to another program for processing and printing. The physicians then have a model of the patient’s vasculature on which they can test the intervention they plan on using.
Adnan Siddiqui, MD and Ciprian Ionita, PhD conceived of using this technology in which a vascular model representing the patient is hooked up to pumps that push liquid through the vessels. “These models offer an environment that is more realistic than that of cadavers where vessels are unnaturally brittle, or that of animals where vasculature is significantly different,” explains Dr. Siddiqui.
Minimally invasive endovascular procedures use the body’s blood vessels to deliver medical devices to the heart or brain to treat heart attacks, strokes, and aneurysms. The 3D vascular flow models created from a patient’s actual imaging make it possible to train medical staff, test medical devices, and help physicians plan minimally invasive endovascular procedures. They are also ensuring that physicians who are performing their first procedures have the skills to do so safely and effectively.
The JI and its partners also use 3D models in clinical immersion programs targeted to medical device company engineers who often create new medical devices in isolation from the clinical environment in which the devices are used. The engineers are able to deploy their medical devices, often for the first time, in the vascular models. With a greater understanding of what it is like to deploy a device inside a patient’s body, it helps them design devices that are easier to use, safer and more effective. Inventors and start-ups from around the world bring their medical device prototypes to the JI for testing in 3D models, and surgeons use patient models to plan and practice complicated procedures before performing them on patients.
The JI was selected by Stratasys to be a 3D printing center of excellence in healthcare. Leveraging a grant of $200,000 from the James H. Cummings Foundation, this partnership includes the acquisition of a Connex3 500 multi-materials printer.
Adnan Siddiqui, MD, PhD, FACS, FAHA is chief medical officer of the JI, and vice chair and professor of neurosurgery at the Jacobs School of Medicine and Biomedical Sciences at UB. Ciprian Ionita, PhD is a research assistant professor of biomedical engineering and neurosurgery in the School of Engineering and Applied Sciences and The Jacobs School of Medicine and Biomedical Sciences at University at Buffalo.
About the Author
Pamela Marcucci, Director for Program Development and Outreach at the Jacobs Institute.