Highly competitive NIH HEAL Initiative issues awards to UB researchers to develop non-addictive painkillers
Researchers in the Jacobs School of Medicine and Biomedical Sciences are using targeted tools to address pain
BUFFALO, N.Y. — A prestigious and highly competitive National Institutes of Health program called the Helping to End Addiction Long-term (HEAL) Initiative, has issued awards to two University at Buffalo faculty members who are studying how to develop novel, non-addicting painkillers.
The NIH HEAL Initiative was launched last year to improve prevention and treatment strategies for opioid misuse and addiction, and enhance pain management. It aims to improve treatments for chronic pain, curb the rates of opioid use disorder and overdose, and achieve long-term recovery from opioid addiction.
This week, NIH announced a total of $945 million in HEAL grants to researchers in 41 states, including those at UB.
Michael E. Cain, MD, dean of the Jacobs School of Medicine and Biomedical Sciences at UB and vice president for health sciences at UB, said the fact that two of the school’s researchers were issued awards is evidence of the caliber of research in UB’s medical school.
“UB is extremely proud that research by our faculty, who are tackling how to develop non-addictive pain treatments—one of society’s most pressing current health issues—is of such a caliber that it has attracted the interest and support of this major NIH HEAL Initiative,” he said.
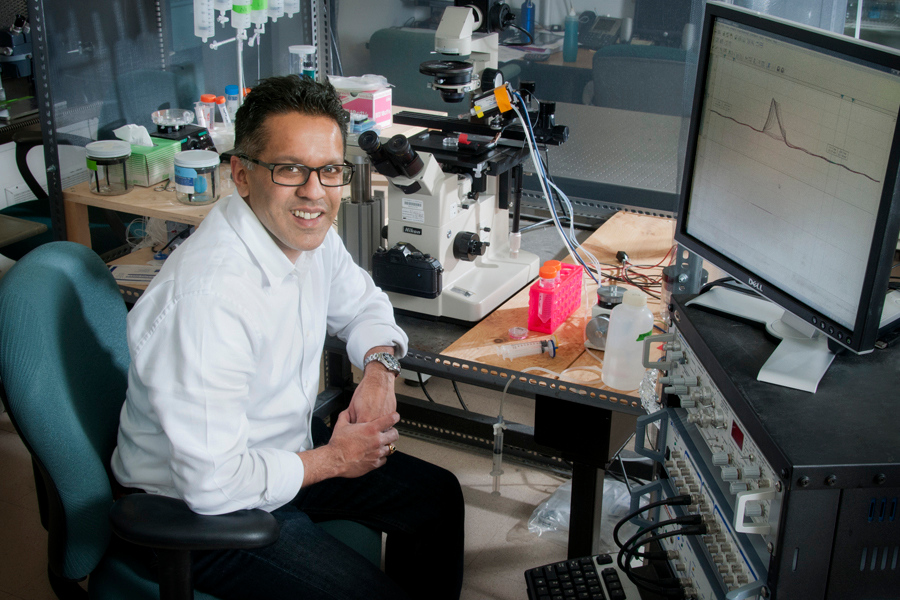
Arin Bhattacharjee, PhD, associate professor in the Department of Pharmacology and Toxicology in the Jacobs School and a faculty member in UB’s Clinical and Research Institute on Addictions, has been awarded $1.9 million for his five-year project on disrupting ion channel scaffolding to treat neuropathic pain.
Tracey A. Ignatowski, PhD, assistant professor in the Department of Pathology and Anatomical Sciences in the Jacobs School and Andrew J. Fabiano, MD, associate professor of neurosurgery and oncology and director of the Spinal Oncology Center at Roswell Park Comprehensive Cancer Center, are also part of the investigative team.
“Our goal is to validate as a novel pain target a type of scaffold protein that regulates key ion channels at the sites of sensory nerve injury,” said Bhattacharjee. He noted that a tremendous amount of pharmaceutical research has focused, unsuccessfully, on drugs that block these ion channels.
“What’s different about our approach is that we think the scaffold protein is bringing ion channels to the area of nerve damage,” he explained.
“We have demonstrated and published that in an animal model, if the scaffold protein is genetically removed or pharmacologically targeted, the sensitivity to pain is significantly decreased,” he said. “The purpose of our grant is to validate that the scaffold protein is the target to go after to address neuropathic pain.”
The team will further validate the analgesic potential of this scaffold protein by conducting studies on isolated human dorsal root ganglion neurons, which are involved in sensing pain, and which will be obtained from consenting patients from whom the neurons are removed as part of their treatment.
Ram Samudrala, PhD, professor and chief of bioinformatics in the Department of Biomedical Informatics in the Jacobs School, is a winner of an ASPIRE Design Challenge prize competition, part of the NIH HEAL Initiative and held by NIH’s National Center for Advancing Translational Sciences.
Samudrala and his teammate, Gaurav Chopra, PhD, of the Department of Chemistry and the Institute for Drug Discovery at Purdue University, won $100,000 for their design solution submitted for Challenge 3: Predictive Algorithms for Translational Innovation in Pain, Opioid Use Disorder and Overdose.
“We have developed the Computational Analysis of Novel Drug Opportunities (CANDO) platform that allows us to screen every drug against every disease by virtually screening every drug or compound against a large library of protein structures,” explained Samudrala, who is also bioinformatics lead for the informatics core of UB’s Clinical and Translational Science Institute.
He said they will use the prize money to extend the platform’s screening in several ways, including screening new compounds not just to see how they interact with proteins, but also against RNA.
The design solution titled Optimum Analgesic Discovery by Multiscale Interactomic Profiling, seeks to virtually design new molecules that are optimal analgesics with a low risk of addiction.
“Our platform will try to look at every gene and every molecule in the body to see how every opiate interacts with every molecule and therefore, to get a comprehensive handle on the puzzle of addiction in the context of pain management,” he said.