Courtesy of Roswell Park Comprehensive Cancer Center Cancer Talk
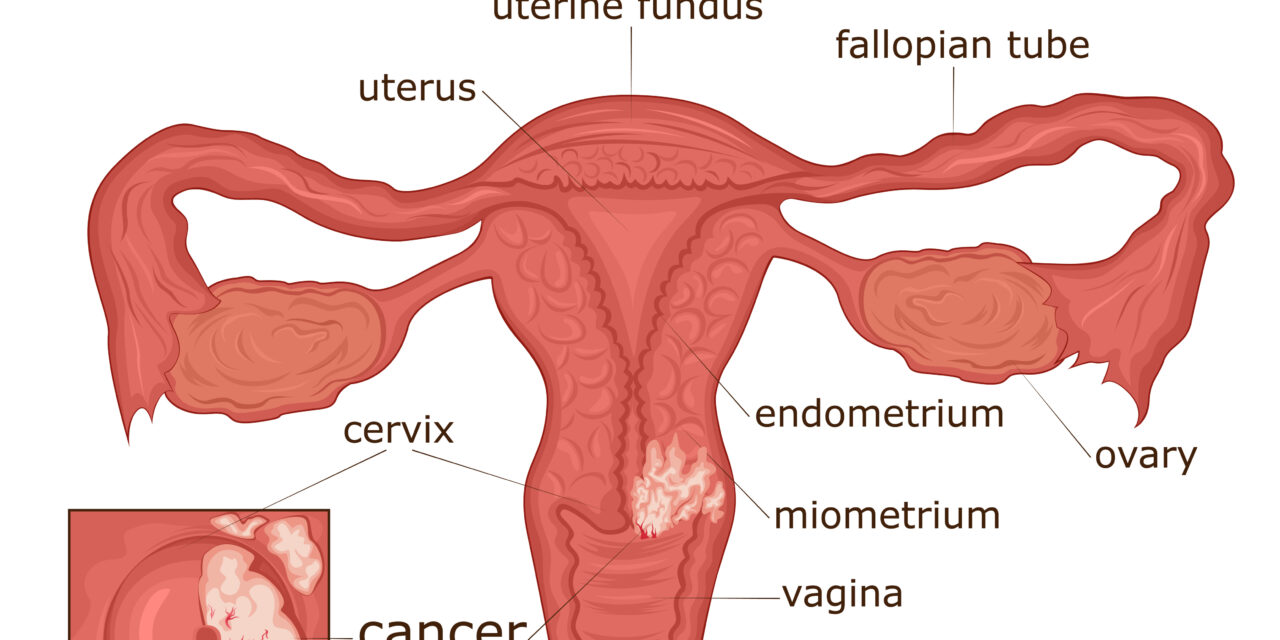
Circumstances surrounding hysterectomies vary. The risk for developing cervical cancer depends upon whether a person’s cervix was removed during a hysterectomy (removal of uterus and cervix), or a supracervical hysterectomy (removal of uterus).
Anatomical factors, such as scarring from endometriosis, may lead a surgeon to perform a supracervical hysterectomy, according to gynecologic oncologist Karen McLean, MD, PhD, Associate Professor of Oncology at Roswell Park Comprehensive Cancer Center. “But overall, removal of the cervix is recommended and standard for women who undergo hysterectomy as part of uterine cancer surgery, for staging and treatment purposes.”
Even if the hysterectomy is being performed for non-cancer reasons, there are benefits to having the cervix removed. “During a minimally invasive hysterectomy, the uterus is removed through the vaginal canal. For this procedure, we have to remove the cervix, or it will block the removal,” says Dr. McLean. Additionally, if a person is undergoing this procedure to treat abnormal bleeding, removing the cervix prevents bleeding afterwards.
Patients who’ve undergone a supracervical hysterectomy still have a risk for developing cervical cancer. “A patient who still has her cervix should continue to undergo cancer screening,” advises Dr. McLean. This includes regular visits to a gynecologist and Pap tests. Your risk for cervical cancer also will depend on your medical history — whether you’ve had abnormal Pap tests in the past, or a history of human papillomavirus (HPV), the virus responsible for most cervical cancers.
The risk of developing cervical cancer following a hysterectomy is much lower for patients who have no cervical dysplasia or precancer cells. However, patients with a history of abnormal Pap tests or HPV may need to continue routine cancer screenings, depending on prior test results.
“There’s a duration after your hysterectomy where you may need to have a vaginal smear,” says Dr. McLean. Like a Pap test, this collects cells from the vagina to test for vaginal dysplasia – skin cells in the vagina that begin to grow abnormally. According to The American College of Obstetricians and Gynecologists, patients with specific Pap test abnormalities prior to their hysterectomy should “continue to have screening for 20 years after surgery.” The need for future testing should be discussed with your gynecologist or primary care provider.
Screening and prevention for cervical cancer can be part of your visit with your primary care provider and gynecologist. Regular Pap tests and HPV tests examine the cervical cells for changes that could lead to cancer over time. If changes are detected, next steps in testing and treatment should be discussed, including the importance of smoking as a risk factor. “Of the things we can change, smoking cessation is huge.”
Persistent infection with HPV is the leading cause of cervical cancer, which is why HPV vaccination is so important. “The goal is total vaccination,” says Dr. McLean “The National Cancer Institute recommends HPV vaccination for all persons, not just women, through age 26, and vaccination has been approved for adults through age 45.” Call 1-800-767-9355 to get screened today.