By Beverly Schaefer, M.D.
Immune thrombocytopenic purpura (ITP) is a blood disorder in which people experience a decrease in the number of platelets in their blood. Platelets are cells in the blood that help stop bleeding, and when there aren’t enough of them, a person can experience easy bruising, bleeding gums, nosebleeds, and heavy menses. ITP is caused by an immune reaction against one’s own platelets. It is very common, and both children and adults can develop the disorder.
Acute immune thrombocytopenic purpura typically affects children ages two through six. Often, the cause it not known, but ITP may occur after a viral illness, such as chickenpox. Most cases are temporary and resolve within weeks or a few months without any treatment being required. Chronic thrombocytopenic purpura can happen at any age, but typically occurs more often in adults and adolescents. Low platelets can persist for a minimum of six months to several years, or even a lifetime, and more females are affected than males. Chronic ITP can recur often, and requires continual follow-up care with a blood specialist (hematologist).
What Causes ITP? Often, there is no known cause of ITP, but it occurs when the body produces antibodies against its own platelets. Also, a type of white blood cell called T-cells directly attack platelets. Although rare, ITP can be triggered by medications that cause an allergy that cross-reacts with platelets; an infection from a virus that prompts antibodies to cross-react with platelets; pregnancy; vaccinations; in conjunction with immune disorders such as rheumatoid arthritis and lupus; and low-grade lymphomas and leukemias that produce abnormal antibodies against platelet proteins.
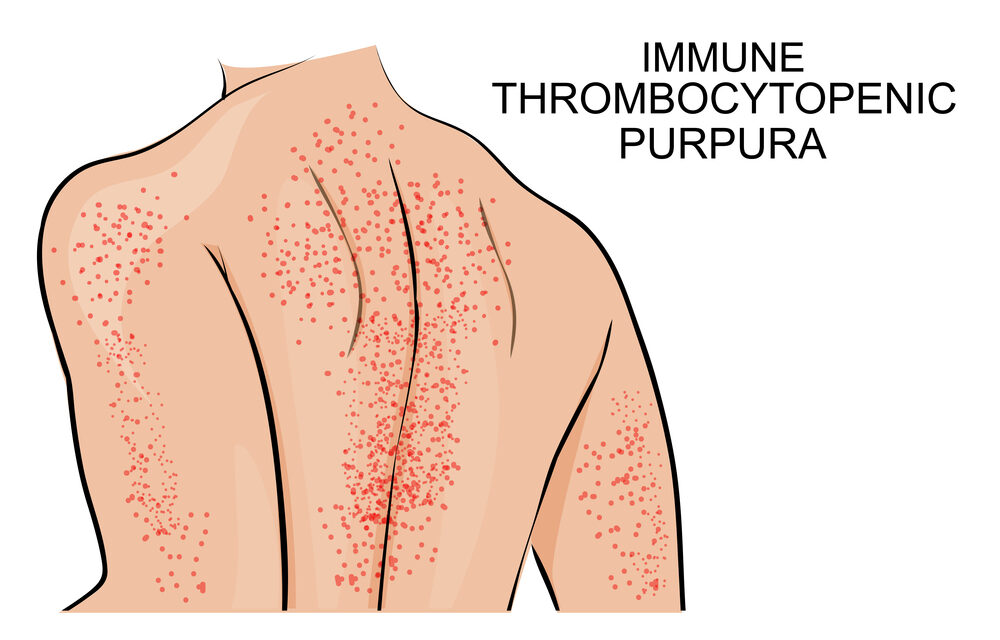
Symptoms of ITP. Our body’s normal platelet count ranges from 150,000 to 450,000. People with ITP have a platelet count less than 100,000. When the platelet count is less than 10,000, more significant symptoms can occur, including extensive bruising; tiny red dots under the skin from small bleeds; nosebleeds; mouth and gum bleeding; heavy menstrual periods; blood in vomit, urine, or stool; and bleeding in the brain — the most dangerous and life-threatening symptom of ITP.
Diagnosing ITP. Diagnosing ITP requires a thorough physical exam, medical history, review of current medications and tests, a complete blood count (CBC), and other blood tests to rule out infections, and identify any associated conditions. ITP is diagnosed after other conditions have been ruled out as low platelets can occur with other health problems.
Treating ITP. Treatment is based on age, overall health, medical history, and severity of bleeding symptoms. There is no cure for ITP. Treatments including steroids, intravenous gamma globulin (IVGG), and Rh immune globulin offer temporary improvement in platelet counts. When ITP occurs due to a medication, the medication may need to be discontinued. When due to an infection, proper treatment of the infection may result in higher platelet counts. There are also immune suppressive medications that slow antiplatelet antibody production and new therapies that stimulate the bone marrow to produce more platelets. Sometimes people must make lifestyle changes by altering their activities to protect themselves from bleeding.
Beverly Schaefer, MD is a non-malignant hematologist, board-certified in both pediatrics and pediatric hematology and oncology. She cares for patients with bleeding disorders and blood clots at the Roswell Park Oishei Children’s Cancer and Blood Disorders Program.